MMR Vaccines and the Anti- Vaccination Movement
News & Politics December 14, 2015By Reneé Scott
Edited by: Cynthia Swisher
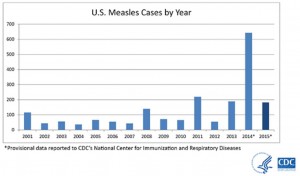 In January of 2015, Disneyland California made headlines when a number of children fell ill after visiting the park. This is a small instance in the overall war on Measles. In 2014, we witnessed the highest number of measles cases in well over two decades.1 This outbreak is due to a detrimental decision made by new parents choosing not to vaccinate their children. Not only does it affect your family, but it can affect your entire community.
In January of 2015, Disneyland California made headlines when a number of children fell ill after visiting the park. This is a small instance in the overall war on Measles. In 2014, we witnessed the highest number of measles cases in well over two decades.1 This outbreak is due to a detrimental decision made by new parents choosing not to vaccinate their children. Not only does it affect your family, but it can affect your entire community.
Measles was deemed exterminated from the United States in early 2000. It has since reemerged due to parents choosing not to vaccinate their children. Measles has reappeared in the US due to unvaccinated residents contracting the virus while traveling overseas and bringing the disease back with them. These contaminated individuals subsequently infect other unvaccinated individuals in their community — placing those too young to be vaccinated as well as those with compromised or weakened immune systems at risk.
Rubeola (measles) is a highly contagious infection caused by a paramyxovirus that targets the respiratory system. It is airborne, and can be fatal in small children. According to the World Health Organization, measles is one of the leading causes of child mortality; worldwide, measles kills over 140,000 people every year. Before the MMR vaccine, measles accounted for approximately 2.6 million deaths each year.4
The MMR (Measles, Mumps and Rubella) vaccine was introduced in 1963.6 By 1981, cases of measles were down by 80% from the previous year. After an outbreak in 1989, physicians began to recommend a follow-up dose of the vaccine. Over the next 20 years, reported cases of the measles declined even further to the point of elimination in the United States. Since the year 2000, the MMR vaccine has prevented an estimated 15.6 million deaths.4
Parents choosing to not vaccinate their children has become a trend in recent years; this fad is called the ‘Anti-Vaccination Movement’. Each year fewer and fewer people are choosing to vaccinate their children. Reasons for opting out of vaccinating may vary but they all boil down to cognitive bias.
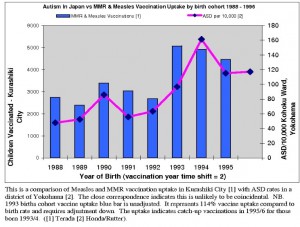 One common misconception is that vaccinations cause autism spectrum disorder. We do not know the precise cause of autism, so we try to attribute the diagnosis to any and every possible source. Early indications of autism tend to present themselves between the ages of 12 to 24 months, at the same time frame the MMR vaccine is recommended (between 12 to 15 months). This is shown further in the bar graph (left) by J Child Psychol Psychiatry2.
One common misconception is that vaccinations cause autism spectrum disorder. We do not know the precise cause of autism, so we try to attribute the diagnosis to any and every possible source. Early indications of autism tend to present themselves between the ages of 12 to 24 months, at the same time frame the MMR vaccine is recommended (between 12 to 15 months). This is shown further in the bar graph (left) by J Child Psychol Psychiatry2.
A report included in Arch Dis Child (2002) attributes the decision to not vaccinate with recall bias:
“Parents of autistic children with regressive symptoms who were diagnosed after the publicity alleging a link with measles, mumps, and rubella (MMR) vaccine tended to recall the onset as shortly after MMR more often than parents of similar children who were diagnosed prior to the publicity. This is consistent with the recall bias expected under such circumstances.”3
Recall bias and correlation only partially explain why parents choose not to vaccinate their children. According to a 1994 study, one main reason for the anti-vaccine trend is due to omission-bias. When faced with the decision to vaccinate, many parents look online for reference. Those who do are sometimes confronted with confusing information. When confused, we are prone to take no action; this is called omission bias. When faced with the idea of either taking an action that could possibly cause harm, or passively not taking an action, which in turn could cause harm, we find it more moral to not take said action although the result would be the same. This leads to parents declining to take the action of immunizing their children.
When weighing the risk of vaccinating against not vaccinating people tend to rely on posts that feed into their cognitive biases. Over the last hundred years people have become dulled the reality of this disease because it is no longer visible. We are not as worried about rubeola for the same reasons we are not frightened of saber-tooth tiger attacks; it just doesn’t seem like a viable threat. People tend to focus so much on the reported risks of vaccinations that they ignore the very real prospect of a recurrence.
1National Notifiable Diseases Surveillance System (NNDSS) and direct report to CD
2J Child Psychol Psychiatry. 2005 Jun;46(6):572-9 (Graph)
3Andrewes, N., E. Miller, B. Taylor, R. Lingam, A. Simmons, J. Stowe, and P. Waight. “Recall Bias, MMR, and Autism.” Arch Dis Child (2002): 493-94. ArchDisChild. 5 Aug. 2002. Web. 20 Oct. 2015.
4 “Measles.” WHO. World Health Orginization, Feb. 2015. Web. 23 Oct. 2015. <http://www.who.int/mediacentre/factsheets/fs286/en/>.
5Asch, David A., Jonathan Baron, John C. Hershey, Howard Kunreuther, Jacqueline Meszaros, Ilana Ritov, and Mark Spranca. “Omission Bias and Pertussis Vaccination.” Omission Bias and Pertussis Vaccination. Med Decis Making, Apr. 1994. Web. 23 Oct. 2015. <http://mdm.sagepub.com/content/14/2/118#cited-by>.
6“Measles History.” Centers for Disease Control and Prevention. Centers for Disease Control and Prevention, 03 Nov. 2014. Web. 23 Oct. 2015. <http://www.cdc.gov/measles/about/history.html>.
Centers for Disease Control and Prevention. “Measles Cases in the United States Reach 20-year High.” ThinkProgress We Thought We Already Eradicated Measles But Thanks To Ongoing AntiVaccine Beliefs Its Back Comments. Centers for Disease Control and Prevention, 13 Sept. 2013. Web. 23 Oct. 2015. <http://thinkprogress.org/health/2013/09/13/2617061/measles-outbreak-vaccine-beliefs/>.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2857525/
Gray, K. & Tonge, B. (2001). Review article. Are there early features of autism in infants and preschool children? J. Paediatr. Child Health, 37, 221-226.
“Vaccines Are Not Associated with Autism: An Evidence-based Meta-analysis of Case-control and Cohort Studies.” National Center for Biotechnology Information. U.S. National Library of Medicine, 17 June 2014. Web. 23 Oct. 2015. <http://www.ncbi.nlm.nih.gov/pubmed/24814559>.
Header photo by IAVI (flickr creative commons)





